Publication Highlight Ann Yates, Gastrointestinal, Evidence & Practice, 2023
This article, written by Ann Yates, director of continence services at St David’s Hospital UK, provides a great tool for HCPs to further understand urinary incontinence and bowel control issues. It shows prevalence numbers, explains the different types of issues, as well as provides continence assessments and how to incorporate these into practice.
What is urinary incontinence?
The term ‘continence’ refers to the ability to effectively self-control urinary functions, and incontinence has been defined as ‘any involuntary loss of urine‘. Incontinence has been shown to negatively affect people’s quality of life as well as mental health. It affects many aspects of everyday life, such as maintaining personal hygiene and the social life. It commonly also leads to skin damage (due to incontinence pads) and pressure ulcers. “Management of incontinence is therefore a central component of quality nursing practice” Ann Yates emphasises.
How many of the population are affected by urinary incontinence?
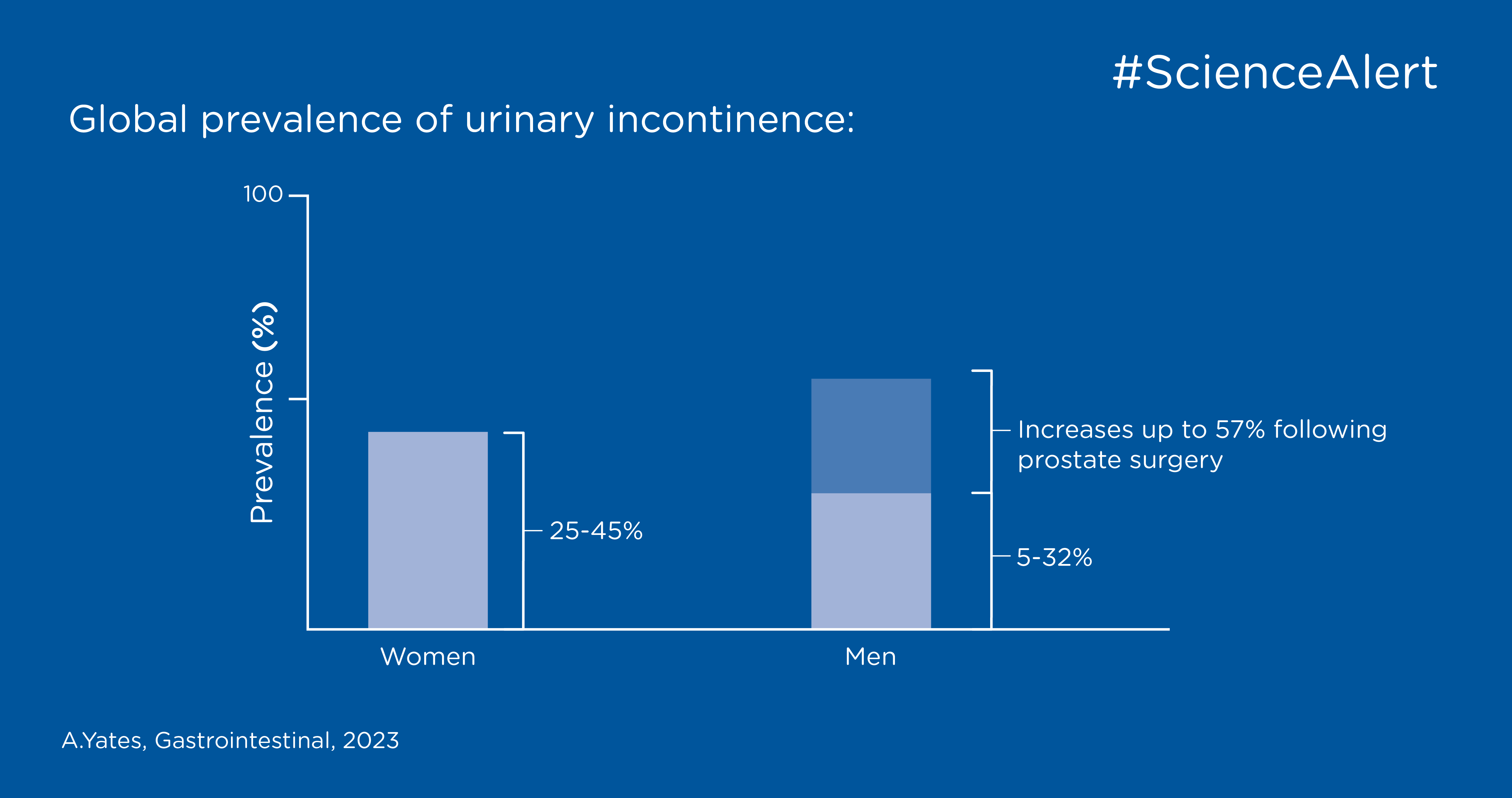
Urinary incontinence is very common worldwide and has been identified as a health priority by the World Health Organization (WHO). The prevalence rates differ between studies, mainly due to the use of different definitions which makes comparisons challenging. Globally, urinary incontinence in women has a reported prevalence of 25-45%. In men urinary incontinence is often caused by previous surgery to remove the prostate and the prevalence of urinary incontinence ranges from 5 - 57 %. For both men and women, the figures increase with age.
What is bowel incontinence?
Bowel incontinence, or faecal incontinence, has been defined as a ‘complaint of involuntary loss of faeces – when faeces is solid and/or liquid’. Although being less common than urinary incontinence, bowel control issues affect as much as 6.5 million people in the UK.
Almost 66% of people who have problems controlling their bowel also experience problems controlling their bladder, this is termed double incontinence. “The prevalence of urinary incontinence and bowel control issues means it is crucial that nurses can recognise and distinguish between different types and be able to assess patients and initiate appropriate treatment, irrespective of specialism or care environment” Ann Yates explains. Furthermore, it’s important to understand that incontinence is considered embarrassing and a taboo subject for many people, which hinders them from seeking assistance and support.

How are the different types of urinary incontinence distinguished?
Stress incontinence refers to the involuntary leakage of urine from the external opening of the urethra in response to increased abdominal pressure. It is associated with a weak pelvic floor and usually occurs after coughing, sneezing, physical exertion, laughing or lifting. This is the most common type in women and mainly related to the effects of childbirth. However, men can also experience this type of incontinence, for example following prostate surgery.
Mixed incontinence is a chronic condition of involuntary urine leakage caused by symptoms of stress and urge incontinence occurring together. Studies have shown that both types of incontinence and symptoms require management to support improvement.
Overflow/obstructive incontinence is associated with various conditions, including pelvic organ prolapse in women and prostate gland enlargement (benign prostate hyperplasia) in men. This type of urinary incontinence can occur as a complication of urinary retention. Besides this, urethral stricture and several different neuropathic conditions (e.g. spina bifida, MS, Parkinson’s disease) can cause overflow/obstructive incontinence. Also, chronic constipation is shown to negatively Impact these symptoms.
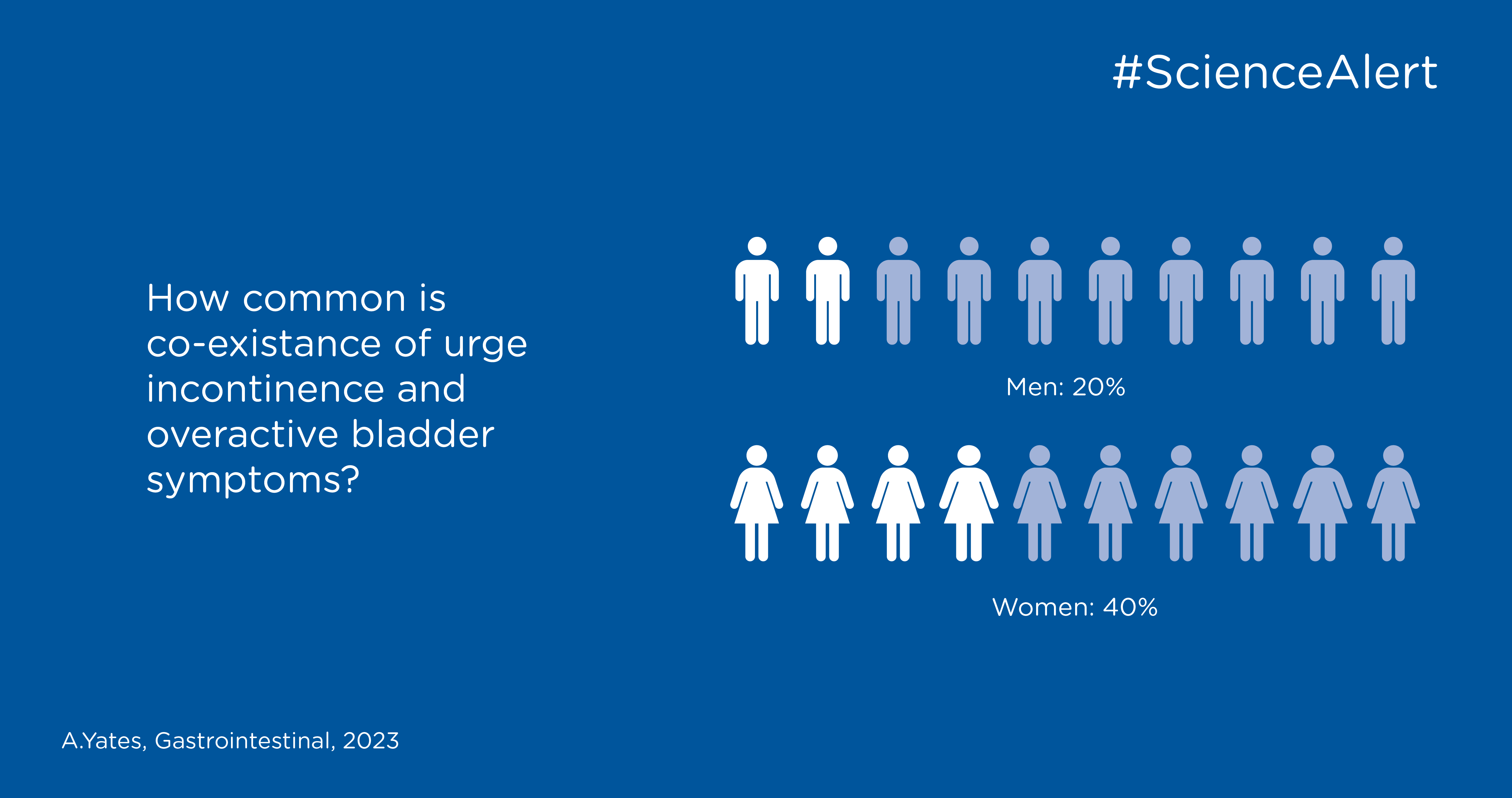
Urge incontinence/ overactive bladder syndrome can be caused by involuntary contractions of the detrusor muscle (in the bladder wall) on bladder filling. The symptoms are often severe with a sudden urge to void which cannot be delayed. Besides urine leakage this type involves nocturia (having to get up at night to urinate). In older people nocturia is shown to have a direct relationship to decreased sleep quality and depression. Urge incontinence has been identified as the most bothersome type by patients.
Patient assessment
The negative effects of urinary incontinence and bowel control issues can be significant, so it is vital that nurses take time to listen to patients and reflect back to them that they have understood their experiences. A basic urinary and bowel continence assessment should aim to identify the following:
Start by collecting the complete medical history of the patient to determine whether the issue is related to a specific event or to a medical condition. The type of bladder and/or bowel problem should be identified; including the symptoms, when they started, as well as their duration. Assess to what extent these symptoms affect the person’s quality of life and how the person manages their symptoms. The patient’s mobility status needs to be examined including dexterity as well as cognitive and social issues. And finally, all types of medications shall be documented together with potential allergies and the person’s body mass index.
Ann Yates writes that: “Although there are no recognised assessment tools for general continence assessment, there are a number of validated tools that can be used to evaluate specific issues, including the following (United Kingdom Continence Society 2015, NHS England 2018):
- The International Consultation on Incontinence Questionnaire (ICIQ) – a patient- completed questionnaire used to evaluate the frequency, severity, and effect on quality of life of urinary incontinence in men and women.
- The St Mark’s Incontinence Score – used to evaluate the severity of faecal incontinence.
- The International Consultation on Incontinence Questionnaire
- Anal Incontinence Symptoms and Quality of Life (ICIQ-B) – a patient-completed questionnaire used to evaluate symptoms of anal incontinence, including flatus incontinence, and effect on quality of life.
Conclusion
Both urinary incontinence and bowel control issues are very common within the general population, therefore nurses in all settings should be able to recognise symptoms, distinguish between the different issues and feel confident to undertake a basic continence assessment. Continence-related issues have a significant negative effect on people’s quality of life and is also associated to embarrassment and people being reluctant to seeking help. Nurses have an important role in helping these people get the help they need based on the individuals’ abilities and circumstances.