Pelvic floor dysfunction (PFD) refers to a broad group of symptoms and anatomical changes related to abnormal function of the structures within the pelvic floor complex, which includes the supportive fibrous tissue called fascia, the blood and nerve supply and in particular the pelvic floor musculature.
This dysfunction may relate to either increased or diminished activity, or inability to coordinate the pelvic floor muscles. Changes regarding the support of pelvic organs are also part of these issues and known as Pelvic Organ Prolapse (POP). The clinical aspects of PFD can be urological, gynaecological, or colorectal and are often interrelated. PFDs are very common and associated with a negative impact on quality of life. The primary aim of this article is to provide a basic understanding of PFD regarding prevalence, risk factors and symptoms as well as available treatment options.
What’s the role of the Pelvic Floor Muscles?
The pelvic floor muscles together form a sort of ‘basin’ or ‘hammock’ to carry and contain the weight of the pelvic organs and maintain their anatomical disposition so that they function normally.
The muscles of the pelvic floor have three main functions:
- Support of the pelvic organs; bladder, urethra, prostate (males), vagina and uterus (females), anus, and rectum, along with the general support of the intra-abdominal contents.
- Contribute to continence of urine and faeces.
- Contribute to the sexual functions of arousal and orgasm.
What is Pelvic Floor Dysfunction?
If the pelvic floor becomes weakened, stretched or traumatised directly, for example at childbirth, this normal support may be lost. This can lead to risk of pelvic organ prolapse (POP; organs visibly protruding), or more commonly to smaller changes in organ position, leading to abnormal function – such as cystocele (bulging of the bladder against the front wall of the vagina and rectocele, bulging of the lower bowel – the rectum, against the posterior wall of the vagina which can cause trapping of stool).
There is not an exact definition of the parameters that constitute a ‘pelvic floor disorder’. Rather, the term is used as a catch-all for a number of conditions that primarily affect the bladder, the lower bowel (anus and rectum) as well as sexual function.
Symptoms of pelvic floor dysfunction include:
- Lower urinary tract dysfunction (LUTS) (urinary incontinence, urgency, voiding dysfunction, feeling of incomplete emptying etc.)
- Lower bowel dysfunction (faecal incontinence, constipation / incomplete emptying, obstructed defecation)
- Sexual dysfunction (erectile and ejaculatory dysfunction, dyspareunia, orgasmic dysfunction)
- Genito-pelvic pain
Pelvic Floor dysfunction may also lead to symptoms of overactive bladder (OAB) which include urinary frequency, urgency, nocturia and nocturnal enuresis.
It’s common that pelvic floor dysfunction leads to several different symptoms. LUTS is commonly associated with constipation as well as urinary and faecal incontinence, and they commonly co-exist.
Sensation of incomplete bladder emptying, and dyspareunia (painful intercourse) is often reported in women with constipation, and these are related to more severe bowel symptoms. For men, LUTS and sexual problems are commonly linked to each other.
Who is affected by pelvic floor dysfunction?
The causes and functional processes of conditions related to PFD are not fully understood. Multiple factors have been discussed, e.g., poor evacuation techniques, lifestyle factors, surgical or obstetric trauma, sexual abuse, irritable bowel syndrome etc. Also, a lot of medications can have a side effect leading to smooth and skeletal muscle relaxation, possibly contributing to incontinence. Symptoms of PFD can stem from urological, gynaecological, and colorectal causes.
Age is one risk factor for pelvic floor dysfunction, obesity and vaginal birth are others, but it is a common misunderstanding that only women are affected and then, only those experiencing trauma at child delivery. As a result pelvic floor dysfunction is mainly studied in females although there are reports that as many as one in eight men have pelvic floor issues.
As the world’s population ages, and we live longer, pelvic organ prolapse is also shown to be a growing concern.
How common is pelvic floor dysfunction?
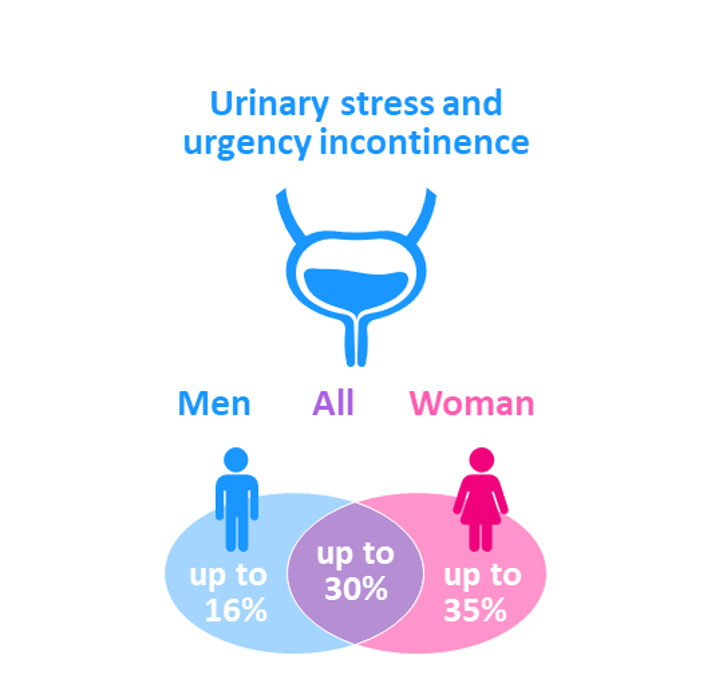
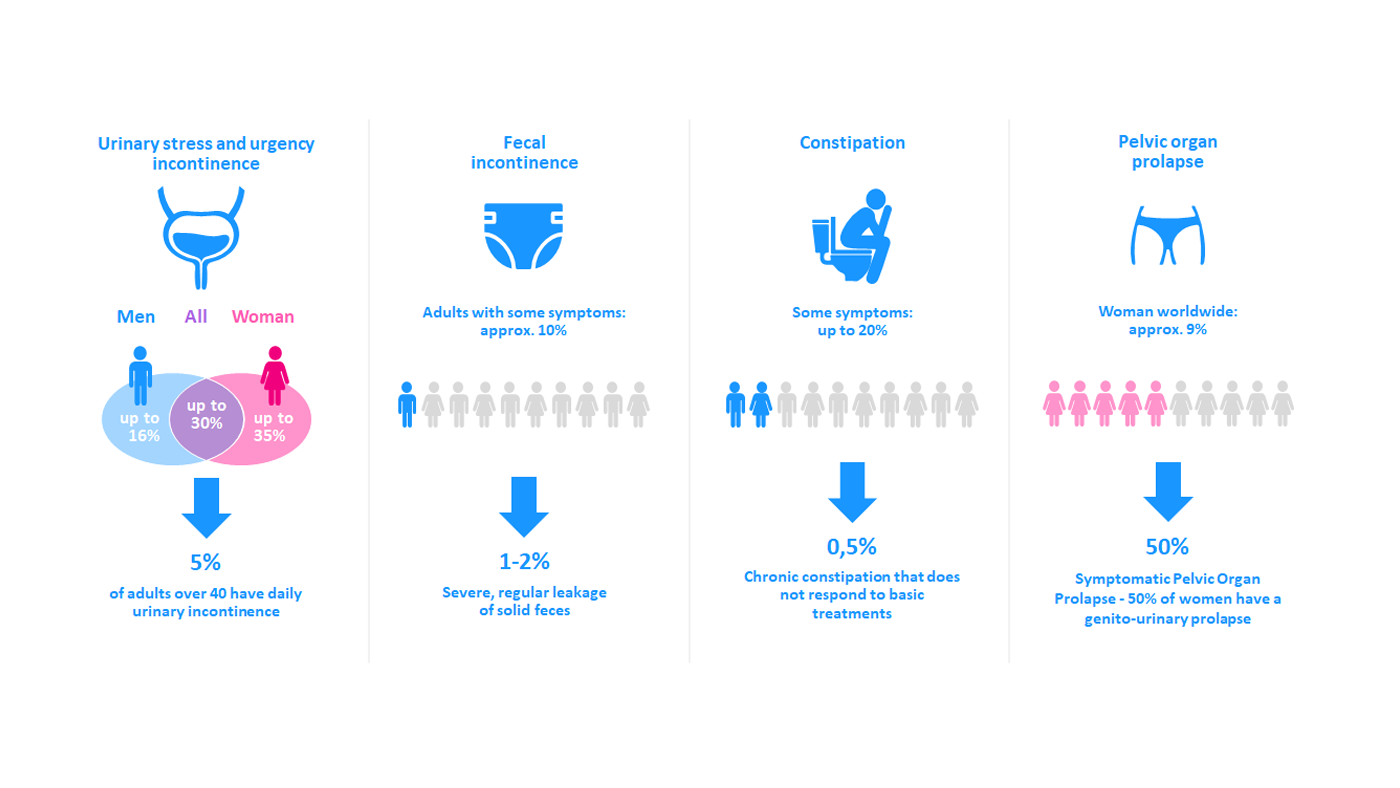
As the symptoms and conditions of pelvic floor dysfunction are broad it’s difficult to determine the overall incidence. However, it’s clear that it is very common for women and even considered a public health issue. But not only women are affected, urinary stress and urgency incontinence disorders have been reported to affect 35% of women and 16% of men.
(The Pelvic Floor Society UK, Pelvic floor report 2021)
Another study reports approximately 32% of the women in the US have at least one pelvic floor dysfunction and the rate more than doubles for women older than eighty years. The most common PFD was bowel dysfunction that was experienced by 25%. It’s also common that patients have multiple symptoms, as noted in a study with 82% of patients with defecatory disorders having multiple urinary symptoms as well.
Why is pelvic floor dysfunction a reason for concern?
The impact of severe pelvic floor conditions on quality of life is huge, and patients can suffer as long as a decade before they reach the right healthcare professional to treat their condition appropriately. Studies show that about 40 % report anxiety and 20% even depression, due to the symptoms caused by pelvic floor dysfunction. Additional studies identified the negative impact on work, where 33% of women reported urinary incontinence to affect their concentration and ability to complete tasks without interruption.
An additional aspect of this is that pelvic floor issues leading to bladder and/or bowel incontinence are considered taboo and often cause embarrassment, to a greater extent than other medical conditions. Not talking about the issues can lead to social isolation which will impact on mental health and wellbeing.
What are the most common management options for Pelvic Floor Dysfunction?
As outlined above pelvic floor dysfunctions are complex and therapeutic interventions should always be tailored to individual specific needs, and often a multidisciplinary approach is needed. Below is a selection of some common management options available.
Lifestyle modifications
- Diet: avoidance of alcohol, caffeine, acidic foods/beverages, concentrated sugar, artificial sweeteners, spicy foods, and cigarettes (related to problems with bladder but also the bowel). Increase fluid and fibre intake (to reduce constipation symptoms)
- Weight loss improves all PFD, for example a 3 - 5% weight reduction can decrease urinary incontinence episodes by about 50%.
- Pelvic floor exercises (Kegel) and core exercises to strengthen the pelvic floor.
Medications
- Topical vaginal estrogen for bladder frequency, urgency, and dyspareunia.
- Anticholinergics for overactive bladder.
- Beta3 agonists for overactive bladder.
- Osmotic or stimulant laxatives to ease symptoms of constipation.
It is important to follow up on both bladder and bowel symptoms since medication used to manage the bladder may affect the bowel, for example anticholinergics can cause constipation.
Surgery
Individualized types of surgery are available to treat the most common conditions: urinary incontinence, cystocele, rectocele and rectal prolapse.
Surgery can often correct the anatomical problem such as the prolapse, but as with all surgery it’s often associated with some degree of risk. As the conditions are common it also leads to long waiting times for surgery in most countries. Often additional pelvic floor care is required after surgery.
Conservative therapy including pelvic floor muscle rehabilitation must always be tried before proceeding to surgery. There is a need to raise awareness of management options for PFD and it is important that patients are informed that non-surgical interventions exist to aid their symptoms.
Intermittent catheterisation and transanal irrigation
Intermittent catheterisation (IC) is considered the standard of care in most neurologic patients with lower urinary tract disorders and is very suitable for increasing quality of life also in patients with PFD. IC mimics the natural way of emptying the bladder and ensures that the bladder is completely empty after the procedure, without leaving any residual urine, which can increase the risk of urinary tract infections as well as urine leakage.
Transanal irrigation (TAI), also called rectal irrigation, is an effective way to ease emptying of the bowel by instillation of water through the anus. For common symptoms of pelvic floor dysfunction such as incomplete evacuation, passive fecal incontinence including post-defecation soiling, and rectocele it is usually enough to use a low volume of water (less than 250 ml) to relief the symptoms and improve quality of life.
In what way may IC and TAI help individuals with PFD?
Many patients are unaware that there are options to treat incontinence and that it should not be accepted as a natural part of ageing, an expected consequence of childbirth, or a typical part of delayed development in children and young people. Studies show that women who are helped by conservative methods skip surgery, since surgical procedures are also associated with risks (especially with mesh insertion). IC and TAI could potentially help these patients take control over their continence issues and improve QoL while waiting.
IC can be an option when a patient has:
- Stress- or urge incontinence
- Problems with urinary tract infections because of incomplete emptying of the bladder
- Urinary leakage which requires pads and is considered inconvenient (smell etc) for the user
- Urinary leakage as a barrier for physical activity
- Anxiety of surgery, or while waiting for surgery
TAI can be an option when a patient has:
- Bowel leakage or fear of leakage
- Pain or pressure in the pelvic region
- A feeling something is left and have an urge to try to empty their bowel often
- A need of rectal or vaginal digitation to assist emptying
- Difficulties to start or finish evacuation or excessive straining during defecation
- A need to use mini enemas with laxatives every day and don’t feel good about it