
Being able to control when you go to the bathroom is important for your health and happiness. Most people will have continence issues at some point in their live but women are more prone to bladder and bowel problems.
These conditions can make a woman's life harder by affecting her health and quality of life. They can make it difficult to do daily tasks, have good relationships, and feel good about oneself. To improve women's health outcomes, we need to understand the factors that cause continence issues. It is important to make sure women have access to the appropriate care.
This guide will talk about the differences in bladder and bowel control in the female body. It will also cover the most common issues that women experience in this area. Next, we will look at key stages in a woman's life when continence issues are more common. We will then explore the various treatment and management options that are available.
Continence and the Female Anatomy
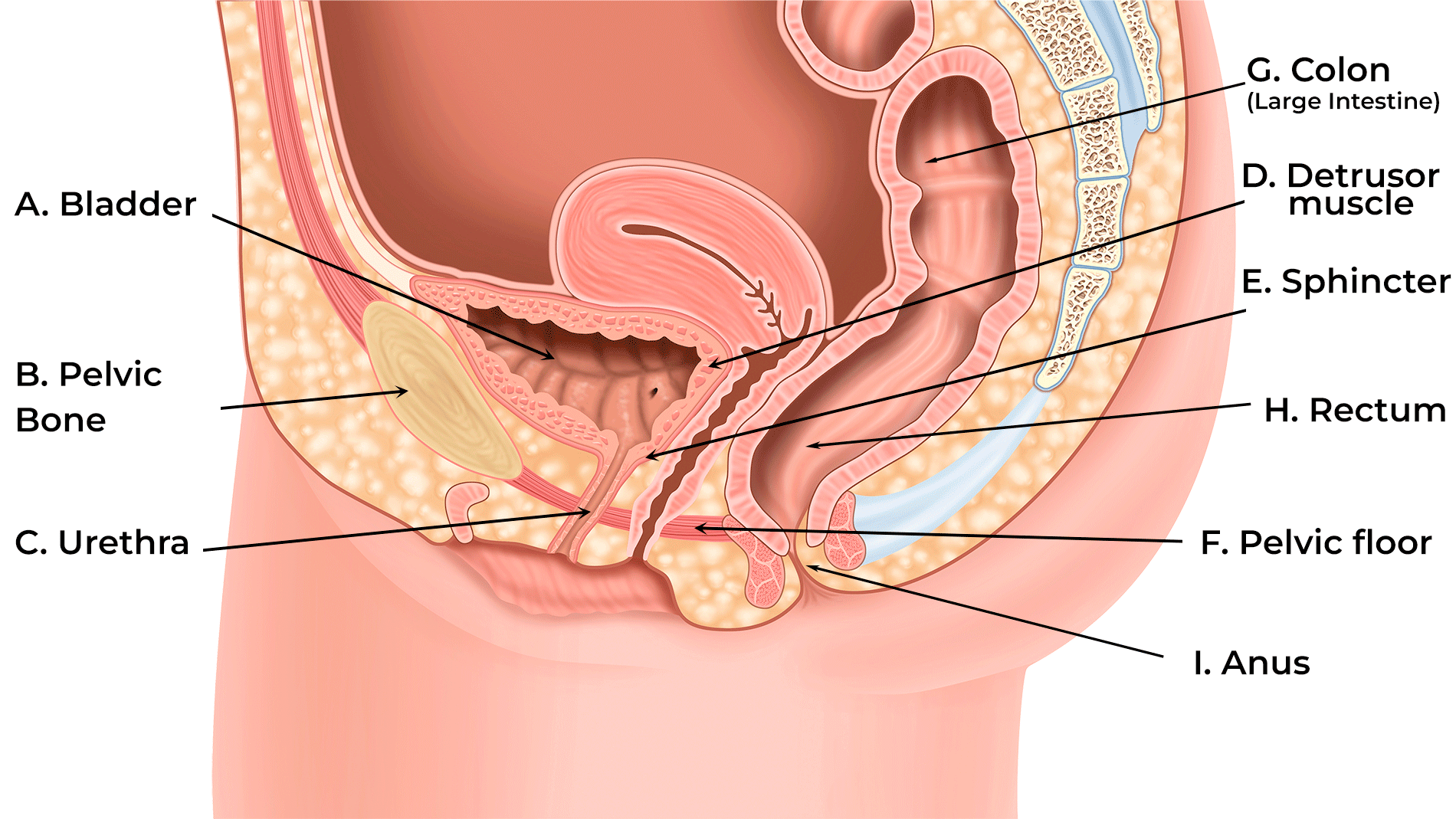
| Label | Description |
| A. Bladder | A storage pouch for urine. A healthy bladder will expand as it fills up with urine and contracts when it's time to empty. |
| B. Pelvic bone | |
| C. Urethra | A tube that carries urine from the bladder out of the body. In females, this is approximately 3-5cm, shorter than in males. |
| D. Detrusor muscle | This is the smooth muscle around the bladder which contracts to help you pass urine. |
| E. Sphincter | These muscles help to open and close your urethra to control the flow of urine. |
| F. Pelvic floor | The pelvic floor is a group of muscles, sometimes likened to a hammock. It supports the organs in a woman’s pelvis, like the bladder, uterus, and rectum. |
| G. Colon (Large Intestine) | Its job is to absorb water and minerals from the digested food that comes from the small intestine. As this happens, the waste material becomes more solid, forming stool (poo). |
| H. Rectum | Imagine the rectum as a storage area, it's where the stool stays until it's ready to leave your body. When the rectum senses that it's time to go to the bathroom, it sends a signal to your brain to let you know you need to go. |
| I. Anus | The relaxing of the muscles around the anus allows you to pass stool out of the body. |
The bladder, urethra, and pelvic floor muscles play crucial roles in maintaining urinary continence. Similarly, the rectum, anus, and pelvic floor muscles are essential for bowel control.
Hormonal changes, pregnancy, giving birth, and menopause can all impact how well these parts work, causing issues with bladder and bowel control. In addition, the proximity of the urinary and reproductive systems and short length of the urethra make women uniquely susceptible to certain continence issues.
What are the most common continence problems for women?
The Most Common Female Bladder Health Issues
Problems related to female bladder health can generally be divided into three main groups; incontinence (leakage), retention (difficulties emptying the bladder) and Urinary Tract Infections.
Urinary Incontinence in Women

Urinary incontinence, the involuntary leakage of urine, is more common in women, occurring 2.5-3 times more often than in men.1 In fact, there are several types of urinary incontinence with some affecting women at an even higher rate.
Stress incontinence happens when the muscles in your pelvic floor or sphincter are weak. It can be triggered by things like coughing, sneezing, or lifting heavy objects. Stress incontinence is three times more common in women because of physical changes that occur during pregnancy, childbirth, and menopause.2
Urge incontinence starts with a strong sensation to empty the bladder. The bladder contracts when it shouldn’t, causing some urine to leak. This type of incontinence is caused by a dysfunction in the bladder. It is common with neurological diseases like Parkinson’s Disease.
Mixed incontinence involves symptoms of both stress and urge incontinence.
Urinary Retention in Women
Women experiencing urinary retention will have difficulty emptying their bladder or may be completely unable to empty their bladder.
Although retention is thirteen times more likely in men than women, it can be much more common following childbirth with 14-20.6% of women experiencing some form of urinary after delivering a child.3
Women may experience retention, especially if they have a neurological disease, prolapse or following surgery. Another potential, although rare, cause of urinary retention in women is Fowler’s syndrome which affects women within the 2nd and 3rd decades of their life.4
Urinary Tract Infections in Females
Urinary Tract Infections (UTI) occur when bacteria have a chance to grow in the urethra and bladder. Like any other kind of infection, the longer it goes untreated, the more serious the complications can be. About half of all women will experience a UTI during their lifetime.
Symptoms of a urinary tract infection in women include:
- Frequent urge to urinate
- Incontinence
- A burning sensation when emptying the bladder
- Blood in urine
- Cloudy, discoloured or smelly urine
- Lower back and abdominal pain
- Fever
- Feeling generally unwell
Women are 3-4 times more likely to get a urinary tract infection than men. Women between the ages of 16-35 are 35 times more likely to get a UTI than men.5 There are several reasons for this:
- Bacteria has less far to travel to reach the bladder as women have a shorter urethra
- The proximity of the vagina and rectum can cause transfer of bacteria during sexual intercourse
- Hormonal changes during pregnancy
- Declining oestrogen levels due to the menopause
If you do get a urinary tract infection, it’s easily treated. Contact your healthcare professional as soon as possible.
The Most Common Female Bowel Health Issues
Similarly, women tend to experience bowel control problems, including faecal incontinence and constipation, at a greater rate than men.
Bowel incontinence in females
Bowel incontinence, also referred to as faecal incontinence or bowel leakage, involves the inability to control bowel movements, leading to unintentional leakage of stool (soiling). 1 in 12 adults worldwide have fecal incontinence. It is more common in women. Fecal incontinence is especially prevalent in older women.6
Common causes of bowel leakage include:
- Constipation – occurring when watery stool passes the hard stool in the bowel
- Neurological diseases such as Multiple Sclerosis
- Neurological damage such as from Spina Bifida
- Changes or damage to the anal canal, rectum or pelvic floor muscles – this is more likely for women as a result of both childbirth and menopause
Constipation in Women
Constipation is when you have trouble going to the bathroom regularly. If this lasts for more than three months, it's called chronic constipation. Again, constipation occurs at a higher rate (2-3 times) in women than in men.7
Depending on the severity of your constipation, you may experience one or more of the following symptoms:
- Lumpy or hard stool
- Bloating or pain in your abdomen
- Straining on the toilet
- Sensation of blockage or obstruction in rectum
- Feeling of incomplete emptying
Constipation can be caused by different factors. These factors include diet, lifestyle choices, and conditions like Multiple Sclerosis (MS) or Spinal Cord Injury (SCI) affecting bowel movements. Women may also experience constipation due to physical or hormonal changes during pregnancy and menopause.
How does continence affect women at different stages of their life?

Pregnancy, Childbirth and Continence
Pregnancy and childbirth exert significant strain on the pelvic floor muscles and surrounding structures. During pregnancy incontinence, both urinary and fecal, is common.
More than half of women report urinary leakage during pregnancy.9 Faecal incontinence is slightly less common with around 40% of pregnant women experiencing some issues.10 In addition, because of hormonal changes during pregnancy constipation is also more common.11
Childbirth, particularly vaginal delivery, can further stretch and damage pelvic floor muscles, increasing the risk of continence problems postpartum.
In a recent webinar, Consultant Physiotherapist Julia Herbert discussed how vaginal childbirth often leads to pelvic floor dysfunction. However, even women who have a caesarean section can experience this issue.
Because the pregnancy itself with the growing weight of the baby and the hormonal changes that women experience in pregnancy can cause dysfunction in the pelvic floor.
Pelvic Floor dysfunction can affect the lower bowel and lower urinary tract. This can cause continence issues mentioned earlier.
Continence and the Menopause
Bladder Issues During Menopause
Menopause brings big changes to a woman's body, especially in hormone levels like estrogen. As a result during and after menopause bladder problems are more likely. Estrogen helps keep the pelvic floor muscles and urethra in good condition. When estrogen levels drop during menopause, the muscles can become less toned and the urethra drier and more fragile.
This weakening can cause urinary incontinence, where women may accidentally leak urine when they cough, sneeze, or do physical activities. During menopause incontinence is common due to weakened bladder support muscles. The condition of the urethra during this time makes recurrent urinary tract infections more likely.
Bowel Issues During Menopause
Alongside bladder changes, menopause can also affect how the bowels work, causing issues with bowel movements. Estrogen helps keep the digestive system running smoothly, but as estrogen levels drop, bowel habits can change.
Again, hormonal changes have many effects during menopause and constipation is a common problem during this time. Lower estrogen levels can slow down how fast food moves through the intestines, making stools harder and more difficult to pass. Additionally, the decrease in estrogen can impact the muscle tone of the pelvic floor, making it harder to poo.
Understanding these changes during menopause is important for managing bladder and bowel issues effectively. By taking care of their bladder and bowel health, women can better manage these changes and keep enjoying their life.
Treating and managing female continence issues
Most women will experience continence issues at some point in their life, especially during pregnancy and menopause. The good news is that there are plenty of options for managing these bladder or bowel problems – no matter the severity.
Treating and managing bladder problems for women
There are many ways to manage bladder problems like urinary incontinence, urinary retention, and UTIs. These can include lifestyle changes or medical treatments. These approaches aim to improve bladder function, alleviate symptoms, and enhance overall quality of life for affected individuals.
Lifestyle Changes
One of the first lines of defence against bladder problems involves making simple yet impactful lifestyle adjustments. These may include:
- Maintaining a healthy weight: Excess weight can put added pressure on the bladder and worsen incontinence symptoms. Losing weight through a balanced diet and regular exercise can help alleviate these issues.
- Diet: Making changes to your diet can help improve your symptoms. Avoiding foods and drinks like caffeine, alcohol, spicy foods, and artificial sweeteners can irritate your bladder and make your symptoms worse. Limiting or avoiding these triggers may provide relief.
- Fluid management: Staying hydrated is important for overall health. However, drinking too much fluid, especially before bed, can lead to nocturia (frequent urination at night). Adjusting fluid intake throughout the day can help manage urinary frequency and urgency.

Medication
In some cases, healthcare providers may prescribe medications to address specific bladder problems:
- Anticholinergic medications: These drugs help relax the bladder muscles and reduce urgency and frequency in individuals with overactive bladder.
- Alpha-blockers: These medications may be prescribed to relax the muscles around the urethra and improve urinary flow in individuals with urinary retention.
- Antibiotics: For UTIs, antibiotics are commonly prescribed to eliminate bacterial infections and alleviate symptoms such as painful urination and urgency.
Pelvic Floor Exercises for Women
Pelvic floor muscle exercises, also called Kegel exercises, can help strengthen the muscles that support the bladder and urethra. These exercises involve contracting and relaxing the pelvic floor muscles to improve bladder control and reduce urinary leakage. A pelvic floor physical therapist can provide guidance on proper technique and tailor exercises to individual needs.
Urinary Incontinence Products for Women
There are various ways to manage urinary incontinence. One option is using absorbent pads. Another option is using pull-up pants. These pants are similar to baby diapers. These products don’t prevent incontinence and are typically recommended for women experiencing mild or moderate incontinence. 12
Female Catheterisation
In cases of urinary retention or incomplete bladder emptying, intermittent catheterisation may be necessary to empty the bladder fully. This procedure involves inserting a catheter into the urethra to drain urine at regular intervals. Clean, sterile technique is essential to minimise the risk of infection and complications associated with catheterisation. Unlike other products for the bladder, using intermittent catheterization can stop urine leaks before they happen, reducing the chance of accidents.
Choosing the right catheter is particularly important for women, especially when it comes to learning the procedure. The female anatomy can make it difficult to see where to insert the catheter, some women find it helpful to use a mirror to help them guide the catheter into place.

Wellspect has designed a catheter to make it simple for women to both learn and perform intermittent catheterisation. To learn more about LoFric Elle click the below:
Treating and managing bowel problems for women
To manage bowel problems like fecal incontinence and constipation, there are different treatments available. These treatments can help improve bowel control and make life easier for people dealing with these issues.
Lifestyle Changes
Making some changes in daily habits can help a lot:
- Eating more fibre: Foods like fruits, vegetables, and whole grains have fibre that helps keep bowel movements regular and prevent constipation.
- Drinking enough water: Staying hydrated makes stools softer, which makes them easier to pass.
- Following a regular bathroom schedule: Going to the bathroom at the same times every day can help train the bowels to be more regular.
Medication
Doctors may prescribe medicines to help with bowel problems:
- Laxatives: These help with constipation by making it easier to have bowel movements.
- Antidiarrheal medications: These can help slow down bowel movements for people who have faecal incontinence.
Bowel Incontinence products for Women
Like with urinary incontinence, some women choose to use pads or pants for fecal incontinence. While these options do not prevent bowel leakage, they can help to absorb fluids and odors.

Another option that can be used to prevent accidental bowel incontinence is the use of a plug or insert. These products are inserted into the anus to effectively block the way for accidental bowel movements. Learn about the Navina Insert below:
Transanal Irrigation
For some women with constipation or other bowel issues, a procedure called transanal irrigation (TAI) might help. TAI is a treatment that helps manage bowel problems. It works by using lukewarm water inserted into the rectum with a special tube.
The water helps move stool out of the body by making the muscles in the bowel work. TAI gives you more control over when and where you go to the bathroom. With an established TAI routine women can completely empty their bowel, preventing accidental leakage or constipation, and will only need to irrigation every 1-2 days.

Depending on the severity of the bowel dysfunction you may wish to use a low-volume irrigation system like Navina Mini or a high-volume system like Navina Irrigation System. Learn about these systems below:
Surgical Intervention
In rare cases where other treatments don't work, surgery might be an option:
- Sacral nerve stimulation: This involves putting a small device near the nerves that control bowel function. It can help improve bowel control for some people.
- Bowel retraining surgery: For severe cases, surgery might be done to fix structural problems in the bowel or to create a new way for waste to leave the body
In conclusion, continence issues are common among women and can significantly impact their physical, emotional, and social well-being. Understanding the factors that can cause bladder and bowel health problems is crucial. Seeking the appropriate care and support is necessary to effectively manage these conditions. It is important to address these issues promptly to prevent further complications. Seeking medical advice and following treatment recommendations can help improve bladder and bowel health.
Healthcare professionals play a crucial role in providing education, assessment, and treatment options to help women regain control and improve their quality of life. By addressing continence issues comprehensively, we can empower women to live actively and confidently.
For Health Care Professionals
-
Pelvic Floor Dysfunction
key:global.content-type: Course
This course will help develop your knowledge about pelvic floor dysfunction, symptoms, risk factors and management of bladder and bowel symptoms.

-
Female Health Course
key:global.content-type: Course
This course is devoted to women. It consists of a selection of articles to develop knowledge around caring for bladder management in women.

-
Women's Bladder and Bowel Health
Deepen your skills about women's bladder and bowel health throughout life's different stages with this joint ISCoS - Wellspect on demand webinar.
Access the webinar (on youtube)
Want to learn more about continence and women's health?
-
Female Bladder Health
Here we look at the importance of female bladder health and the reasons women are more prone than men to get UTIs.

-
Female urinary incontinence: symptoms, diagnosis & treatment
key:global.content-type: Article
Female urinary incontinence is a very common condition. It affects 1 in 4 women and means an involuntary loss of urine. As well as the physical effects of the condition, frequent accidents can lead to social discomfort or isolation. Let's take a look at what everyday life entails with respect to recognising and treating this issue, how can we recognise it and what solutions and treatments are available.

-
3 Most Common Female Bladder Problems
A burning sensation, sprints to the bathroom or just a little dribble? Symptoms from the lower urinary tract (LUTS) are extremely common in women, but nevertheless both unpleasant and embarrassing.

-
Pelvic Floor Dysfunction
key:global.content-type: Article
Pelvic floor dysfunction (PFD) refers to a broad constellation of symptoms and anatomical changes related to abnormal function of the structures within the pelvic floor complex, which includes the supportive fibrous tissue called fascia, the blood and nerve supply and in particular the pelvic floor musculature.
